November is Diabetes Awareness Month, and that means it’s time to talk about how diabetes impacts eye health.
What is diabetic eye disease?
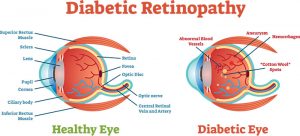
Diabetic eye disease is a group of three eye conditions. Diabetic retinopathy happens when high blood sugar causes vessels in the retina to swell and leak, distorting vision. As it advances, new blood vessels grow on the retina, causing scarring and cell loss. Cataract is when the lens of the eye is clouded. Glaucoma is a group of diseases that damage the optic nerve and can cause vision loss and complete blindness.
Which is most common?
Diabetic retinopathy is the most common, and it is the leading cause of blindness in people with diabetes and all working-age adults.
What are the stages of diabetic retinopathy?
-
Diabetic Retinopathy by AOA Mild nonproliferative retinopathy: Microaneurysms, tiny areas of swelling in the blood vessels form and may leak.
- Moderate nonproliferative retinopathy: The blood vessels that nourish the retina swell and may stop transporting blood. This can actually change the way the retina looks and cause fluid buildup in the macula, which is key to sharp central vision. This is called diabetic macular edema.
- Severe nonproliferative retinopathy: More vessels are blocked, and the areas that are deprived of blood signal the retina to grow replacement vessels.
- Proliferative diabetic retinopathy: New, fragile blood vessels grow inside the retina and the fluid inside the eye, and then start to leak. Scar tissue created during this process can cause the retina to detach from the back of the eye, leading to permanent vision loss.
Who is at risk to develop diabetic eye disease?
Anyone who has diabetes—type 1 and type 2—can develop diabetic eye disease. Your chances increase the longer you have diabetes. More than half of all people with type 1 diabetes develop retinopathy after a decade; nearly 1/3 of people with type 2 already have it by the time they are diagnosed with diabetes. People who have or develop diabetes during pregnancy can experience rapid onset or worsening of diabetic retinopathy.
What are the symptoms of diabetic retinopathy?
There are often no symptoms in the early stages. Most people first notice when it begins to impact their vision. You may see spots that appear to float across your field of vision; these are caused by the bleeding. And fluid retention in the macula, called diabetic macular edema, causes blurred vision.
How is diabetic retinopathy diagnosed?
A comprehensive eye examination that includes the dilation, or widening, of the pupils using drops is the best way to diagnose diabetic retinopathy. Your eye care professional may also test the pressure inside your eye, use optical coherence tomography to grab images of the tissues inside your eye or perform a fluorescein angiogram to identify damaged blood vessels.
Is there any way to prevent diabetic retinopathy?
Early detection and subsequent treatment reduces your risk of blindness by a whopping 95 percent. That’s why it’s important for people with diabetes to have regular comprehensive eye exams at least annually. Those with early stages of diabetic eye disease need to have exams more frequently, and people with diabetes who become pregnant should have an exam immediately. Keeping your diabetes under control is also key; research shows that people who keep their blood sugar level close to normal are significantly less likely than others to develop diabetic retinopathy. You should also take your medications as prescribed, maintain a healthy weight, exercise daily, control your blood pressure and cholesterol, and don’t smoke.
How is diabetic retinopathy treated?
Some vision loss caused by diabetic retinopathy is irreversible, but early detection and treatment significantly increases the chances of saving your eyesight. Your eye care professional can use focal/grid macular laser surgery to slow fluid leakage or scatter laser surgery to shrink new blood vessels. They can also inject medication into the eye—anti-vascular endothelial growth factor injection therapy—to reverse new blood vessel growth and prevent leakage. In vitrectomy, doctors surgically remove some of the gel that fills the eye, solving the problem of bleeding in that area.
What should I do if the treatments don’t restore my vision?
Talk to your doctor about low vison and rehabilitation services, which can provide tools, counseling, training and other services that help you make the most of your remaining vision.
Schedule an appointment for a comprehensive eye exam with a University Eye Center doctor today!